 Reuters
Reuters
The Health and Social Care Secretary Wes Streeting says the government has already cut NHS waiting lists by almost 160,000 since July.
“As we work to end the misery of people left stranded on NHS waiting lists, we will also continue to address the issues facing our A&E departments,” he says.
“Annual winter pressures should not automatically lead to an annual winter crises.”
The government will soon be publishing a plan to improve urgent and emergency care services, he says.
 Nick Triggle
Nick Triggle
Health correspondent, reporting from the Royal Free Hospital
The Royal Free Hospital is under significant pressure this
morning.
The NHS uses what is called operational pressures escalation
levels (Opel) to monitor every site.
The Royal Free is at a high three – one level below the
highest alert level four.
At level four, steps such as diverting patients to nearby
hospitals are considered.
Staff here say it will not take much to push the hospital to
that point.
There is no space left in A&E and there are some
patients who are in trolleys or on chairs outside wards waiting for a bed.
Moving up to level four is not that unusual for hospitals
during recent winters. But it is a sign of just how bad the strain is at the
Royal Free at the moment.
 Hugh Pym
Hugh Pym
Health editor, reporting from the Royal Free Hospital
A
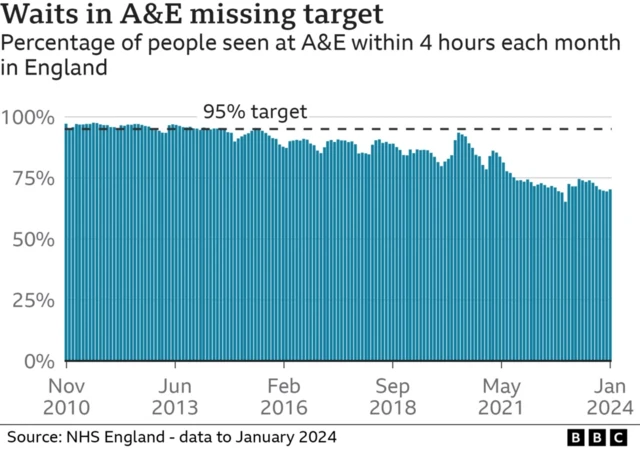
key benchmark for A&E performance in England showed a slight improvement in
January – with 73% of patients treated or assessed within four hours. But
that was still well short of the 95% target.
Ominously
the numbers enduring long waits went up in the month, with nearly 160,000 waiting
longer than four hours for a bed to be found after a decision to admit them – many
on chairs or trolleys.
Over 54,000 waited longer than 12 hours in emergency
departments before a bed was found.
At first glance these numbers look
like the highest since records began.
 Your Voice, Your BBC News
Your Voice, Your BBC News
Bobbi Huyton
 Handout
Handout
Jairo in Chester tells Your Voice, Your BBC News that his 74-year-old mother-in-law faced agonising waits for a bed at a north-west England hospital, when she was suffering with pneumonia.
He says, “many others were in the same situation. The conditions inside the hospital were unbelievable – all of the corridors were full of people being attended in chairs or on trolleys.
“A ward for two people would have around ten people within it. Staff were very apologetic about the situation. It was a traumatic experience.”
As a reminder, you can get in touch with your experience of the NHS via email [email protected], WhatsApp +44 7980 682727 or by clicking here.
 Michelle Roberts
Michelle Roberts
Health editor, BBC News online
Here’s some more key points from the latest NHS statistics which were released this morning:
- The NHS delivered more than 28.3 million tests and checks in 2024 – up a fifth on 23.6 million in 2019 and up 7% on 26.5 million in 2023
-
NHS staff delivered 2.24 million checks in December alone, up 21% on 1.85 million in 2019
-
The NHS met the faster diagnosis standard for cancer again in December with 78.1% of people receiving the all clear or a definitive diagnosis
-
There were 20,000 more people diagnosed or given the all clear within the standard compared to the same month in 2023 – 190,571 in December 2024
-
Despite high levels of winter illnesses like flu and norovirus, high bed occupancy and difficulties discharging patients, 73% of patients were seen within four hours in A&E – an improvement on the month before and the same month in 2023
Professor Julian Redhead, NHS England’s national clinical director for urgent and emergency care, says the figures “show how innovations and the hard work of staff is now delivering consistent progress in bringing down the backlog”.
“This post pandemic period is potentially the hardest the NHS has ever managed and that has certainly been true this winter with soaring levels of viruses, high bed occupancy and difficulties discharging patients,” he adds.
Despite this, A&E and ambulance waiting times were improved, Redhead says.
The public can help by only using 999 in a life-threatening emergency and 111 for other conditions.
 Nick Triggle
Nick Triggle
Health correspondent, reporting from the Royal Free Hospital

Senior staff nurse Greg Kite spoke to me a little earlier this morning after finishing his 12-hour
night shift working in the resus areas of Royal Free’s A&E. This is for the
most seriously unwell patients who need close monitoring.
“It was pretty busy – in resus we had to provide care to 12
patients. But there was good flow through the rest of the departments, although
in the minors side there were nine-hour waits to see a doctor.”
Some of his patients had conditions such as
heart failure, which was causing breathing difficulties, as well as two
patients who staff were worried could develop sepsis, a potentially
life-threatening immune reaction to an infection.
“We are on alert for that. We quickly carry out tests
because any delays treating can have serious consequences.”
 Michelle Roberts
Michelle Roberts
Health editor, BBC News online
More now from the new figures from NHS England.
It shows an average of 14,087 beds were taken up by patients who were medically fit for discharge each day last week, the highest so far this winter.
That’s around one in seven.
The previous week it was 13,776.
But, on planned treatment waiting lists, the overall backlog has dropped again, from 7.48 million to 7.46 million, while the estimated number of patients waiting is down from 6.28 million to 6.24 million.
The proportion waiting less than 18 weeks was 58.9%, up from 56.6% in December 2023.
The number waiting more than a year is now 2.7% of the waiting list, the lowest proportion since August 2020.
The Royal Free Hospital is currently running under its full capacity protocol.
One patient has been waiting for 24 hours to get a ward bed.
Take a look inside:
 Nick Triggle
Nick Triggle
Health correspondent, reporting from the Royal Free Hospital
We’ve just received an update from Peter Hollely, the senior
matron in A&E.
He says the unit is full, there’s no cubicles free now and they
have 20 patients waiting for a bed on a ward.
“It will not take much to tip us over. We’ve not yet been
forced to start corridor care, but it could happen.”
This was something that the Royal College of Nursing
recently warned about with hospitals across the country being forced to set up
make-shift areas for patients.
Peter has just come from a hospital-wide meeting with senior
staff where they had discussed the pressures across the site.
“We had a busy day yesterday – nearly 400 patients came into
the emergency department and that has had a knock-on impact today.”
There are a number of patients who have been moved away from
A&E and placed in what is known as a boarding situation. This means they
are in treatment rooms and side rooms outside wards waiting for a bed to become
free.
“It’s about balancing risk,” he says.
“It’s not ideal, but
it means we can relieve some of the pressure in the emergency department.”
We will be checking back in with Peter throughout the day.
 Hugh Pym
Hugh Pym
Health editor, reporting from the Royal Free Hospital
A quick
read of the latest NHS England stats shows overall waiting just for planned
treatment fell in December for the 4th month in a row to 7.46 million – the
peak was 7.7 million in 2023.

While we let out correspondents pore over the newly-released waiting time figures from NHS England, let’s bring you some comments that Peter Landstrom, group chief executive of Royal Free London NHS Foundation trust, made in the last hour.
Landstrom says the biggest challenges the trust is facing are demand on the emergency department, long waiting lists, and the growing number of cancer patients.
Coping with these demands “whilst also trying to think differently” and create innovations – “that balance is probably the most tricky thing”, he tells the BBC Radio 4’s Today programme.
On AI, he says it has “huge potential” to transform how NHS patients and staff interact.
“The heart of the NHS is its people,” Landstrom says, and they give everything they can, but they work very hard.
AI can therefore be used to “improving our productivity and our efficiency”, Landstrom explains.
He gives the example that AI can plan treatments for a patient in one hour, as opposed to the eight it would take a consultant.
The NHS have just published the newest statistics on patient waiting times for the winter period.
We’re now taking a look at the figures. Stick with us as we bring you the key takeaways.
 Family handout
Family handout
A BBC
Breakfast viewer, Louise, has sent through an image from
a hospital in North West England.
Louise says her 88-year-old nan Maureen was
admitted on Monday and has been in a corridor in A&E for more than
50 hours despite being on the priority list.
We’re following up on her story and will have more details soon.
 Nick Triggle
Nick Triggle
Health correspondent, reporting from the Royal Free Hospital
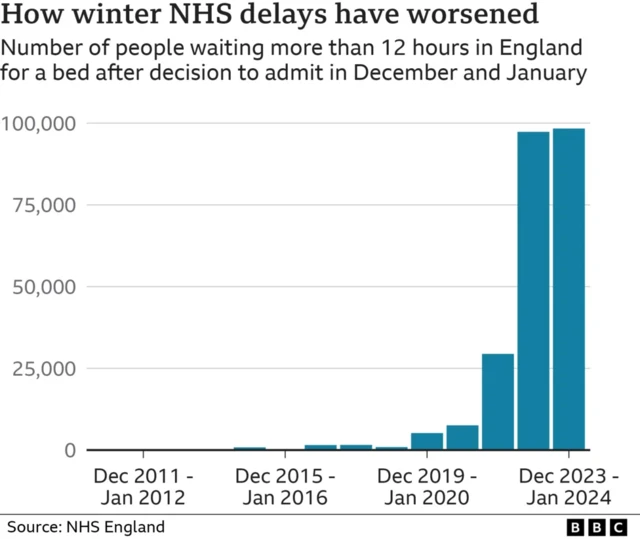
The number of patients waiting more than 12 hours for a bed on a ward after being seen in A&E in England was 19 times higher this winter than it was before the pandemic, figures show.
There were nearly 100,000 12-hour waits in December and January – compared with slightly more than 5,000 in 2019-20.
A decade ago these waits were virtually unheard of – in the four winters up to 2013-14 there were fewer than 100.
The King’s Fund said long delays were at risk of becoming normalised.
It said the pressures this winter had received little attention compared with last winter, despite no significant improvement in performance.
During December 2023 and January 2024, 98,300 patients waited more than 12 hours for a bed on a ward after A&E doctors took the decision to admit them.
These tend to be the sickest and frailest patient – and this wait comes after they have already waited to be seen in the first place after arriving at A&E.

Your Voice, Your BBC News was launched to give our audience – you – more of a say in what we cover and to be part of the news.
Health and the NHS are consistently among of the top topics you want to talk about, making up around one in ten of the responses we get.
Among them, hospital services – from waiting times for referrals to the care patients receive – regularly come up as concern.
We want you to tell us your experiences of hospitals – good as well as bad – whether you are a patient or an NHS staff member.
You can email [email protected], WhatsApp +44 7980 682727 or click here.
 Nick Triggle
Nick Triggle
Health correspondent, reporting from the Royal Free Hospital
 PA Media
PA Media
The Lib Dem leader, Ed Davey, says the crisis in the NHS stems from issues within the social care system.
“The scenes in hospitals this winter have been frankly
horrifying, with patients dying in corridors and staff at breaking point. This
crisis stems from a broken social care system, with thousands stuck in hospital
beds because they can’t get the care they need,” he tells me.
“It is bitterly disappointing that the government
has kicked the can down the road on social care yet again.
“We need to see the government’s social care review
finished within a year at the most, this winter has shown patients cannot
afford to wait another three years for action.”

Dr Khai Lee Cheah, a consultant who works with geriatric patients at the hospital, says the hospital can be under “a lot of pressure” as the discharge of healthy patients has been “quite challenged”.
She gives the example of an 84-year-old man, who had his door broken in by the fire brigade when he needed medical care. He can’t go home now because the door isn’t fixed yet, and so he is taking up a bed.
Cheah says issues like this are “not uncommon”, and access complexities often crop up.
She says it can be challenging at the hospital, but “we all do our best to ensure that they [patients] get compassionate and good care and that they go home when they are ready to go home”.
Looking to the future, she says “things are challenging but they’re not bleak”.
 Reuters
Reuters
Before 2024’s General Election, Labour said that “as a first step”, they would deliver an extra 40,000 operations, scans and appointments a week in England – two million a year. The plan represented an increase of less than 2%.
Labour’s manifesto also said they would “use spare capacity in the independent sector to ensure patients are diagnosed and treated more quickly”.
Among other pledges, they promised to “double the number of CT and MRI scanners” and, in dentistry in England, “provide 700,000 extra appointments each year”.
In December, Labour reaffirmed its plan to have 92% of patients begin hospital treatment or be given the all clear within 18 weeks, by the end of this parliament (2029).
This has been an official NHS target for some time but has not been met since 2015. Currently, around 60% of patients meet the 18-week target.
As a reminder, new NHS data is coming out after 09:30 GMT – we’ll go through it all on this page.
 Hugh Pym
Hugh Pym
Health editor, reporting from the Royal Free Hospital
Head
of NHS England Amanda Pritchard has told BBC Radio 4’s Today programme that private
investment in NHS buildings and equipment may be required.
In comments which go
further than before she said: “We need to think
much more radically, particularly about capital.
“So I think we now must
consider private capital investment in the NHS because if we don’t fix our
buildings, if we don’t fix our technology we’re not going to get to a place
where we can really drive that long term improvement,” she told the programme.

Amanda Pritchard, chief executive of NHS England, says the secretary of state has been clear “there are not overnight fixes” for the NHS, but she is “hugely pleased” that work has been commissioned into social care.
We brought you some of her comments earlier, but now speaking to BBC Radio 4’s Today programme, she says “rather than doing something fast, actually the most important thing is to do it right”.
The government has announced that Louise Casey has been appointed to head an independent commission into reforming social care.
On funding, “we take the responsibility to spend public money wisely very seriously,” Pritchard says. “We need to make absolute best of the money that we’ve got.”
But to provide high quality care, they need “high quality buildings” and technology, she says.
However, she adds, they cannot keep asking the government for more state funding, and “now must consider private capital investment in the NHS”.














